Hypertension secondary to primary malignant neoplasm of the brain represents a complex clinical scenario where elevated blood pressure develops as a direct or indirect consequence of intracranial malignancy. This condition poses significant diagnostic challenges and requires careful consideration in both clinical management and medical coding practices. The interconnection between brain tumors and cardiovascular regulation involves multiple mechanisms, including mass effect on brain structures, increased intracranial pressure, and neuroendocrine disturbances that can disrupt the body’s natural blood pressure homeostasis. Understanding this relationship is crucial for healthcare providers, medical coders, and patients alike, as it influences treatment decisions, prognostic assessments, and accurate documentation of the patient’s condition.
The coding of this condition requires careful consideration of ICD-10-CM guidelines to ensure accurate representation of the cause-effect relationship between the brain tumor and the subsequent development of hypertension. Proper coding not only facilitates appropriate reimbursement but also contributes to valuable epidemiological data that can advance our understanding of this complex comorbidity. This article explores the intricacies of coding hypertension due to primary malignant neoplasm of the brain, providing comprehensive information for healthcare professionals navigating this challenging clinical scenario.
Understanding the ICD-10 Coding Challenge
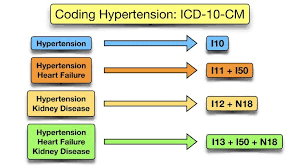
Coding hypertension resulting from a primary malignant brain neoplasm presents unique challenges within the ICD-10-CM system. Unlike essential hypertension (coded as I10), which has no identifiable cause, hypertension secondary to a brain tumor falls under the category of secondary hypertension . However, the ICD-10-CM index does not provide a direct code for hypertension specifically caused by brain neoplasms, creating a coding dilemma that requires careful application of coding guidelines and clinical knowledge.
The complexity arises from the need to accurately represent both the malignant brain tumor and its hypertensive manifestation while respecting the hierarchical structure of the ICD-10-CM classification. Coders must determine whether the hypertension is truly a consequence of the brain tumor or merely a coincidental comorbidity. This distinction requires thorough review of clinical documentation, including physician notes, imaging studies, and laboratory results. The coding challenge is further compounded when the brain tumor affects regions responsible for blood pressure regulation, such as the brainstem or certain cortical areas, leading to direct neurogenic hypertension rather than secondary hypertension through other mechanisms like renal compression or endocrine disturbances.
Primary ICD-10 Codes for Hypertension and Brain Neoplasms
Essential Hypertension (I10)
Code I10 is used for essential (primary) hypertension without identified cause, but it may be inappropriate when hypertension is directly caused by a brain tumor . This code includes various hypertension types but excludes those complicating pregnancy or involving specific vessels . The code I10 represents a billable/specific ICD-10-CM code that can be used for reimbursement purposes, effective for the 2025 fiscal year starting October 1, 2024 .
Malignant Neoplasm of Brain, Unspecified (C71.9)
Code C71.9 classifies malignant neoplasm of brain, unspecified as a billable/specific ICD-10-CM code . This code encompasses various types of primary brain cancers without specification of exact location within the brain, including:
- Glioblastoma multiforme
- Astrocytoma of different grades
- Malignant glioma
- Ependymoma
- Oligodendroglioma
- Primitive neuroectodermal tumors (PNET)
It is crucial to note that C71.9 specifically refers to primary malignant neoplasms of the brain, not metastatic lesions from other primary sites .
Secondary Hypertension (I15 Series)
The I15 code series captures secondary hypertension resulting from underlying conditions . While no specific code exists for brain tumor-induced hypertension, these codes may be applicable depending on the mechanism:
- I15.0: Renovascular hypertension
- I15.1: Hypertension secondary to other renal disorders
- I15.2: Hypertension secondary to endocrine disorders
- I15.8: Other secondary hypertension
- I15.9: Secondary hypertension, unspecified
For brain tumor patients, I15.9 might be used when the hypertension is clearly documented as secondary to the neoplasm but doesn’t fit other specific categories .
Table: ICD-10 Codes Relevant to Hypertension and Brain Neoplasms
| ICD-10 Code | Description | Type | Billable |
|---|---|---|---|
| I10 | Essential (primary) hypertension | Primary hypertension | Yes |
| C71.9 | Malignant neoplasm of brain, unspecified | Malignancy | Yes |
| I15.9 | Secondary hypertension, unspecified | Secondary hypertension | Yes |
| I67.4 | Hypertensive encephalopathy | Complication | Yes |
Coding Hypertension Due to Primary Malignant Brain Neoplasms
Official Coding Guidance
According to ICD-10-CM guidelines, when hypertension is documented as being due to a primary malignant brain neoplasm, coders should assign:
- C71.9 for the primary malignant brain neoplasm
- I15.9 for the secondary hypertension
The sequencing of these codes depends on the reason for the encounter. If the encounter is primarily for management of the hypertension, the hypertension code may be sequenced first. If the encounter focuses on cancer treatment, the neoplasm code should be sequenced first, followed by the hypertension code.
Documenting the Relationship
Clinical documentation must clearly establish the cause-effect relationship between the brain tumor and hypertension. Physicians should specify phrases such as:
- “Hypertension secondary to brain neoplasm”
- “Hypertension due to increased intracranial pressure from brain tumor”
- “Neurogenic hypertension caused by mass effect of primary glioblastoma”
Without explicit documentation linking the two conditions, coders may need to assign codes for both conditions without implying a relationship, which could lead to incomplete representation of the clinical picture and potentially affect reimbursement.
Handling Hypertensive Emergencies
In cases where the hypertension becomes severe and leads to hypertensive emergencies with brain tumor patients, additional codes may be required:
- I16.1: Hypertensive emergency
- I67.4: Hypertensive encephalopathy (if applicable)
Hypertensive encephalopathy is a particular concern in brain tumor patients, as the combination of compromised cerebral autoregulation and acute blood pressure elevation can lead to significant neurological deterioration .
Pathophysiological Mechanisms Linking Brain Tumors to Hypertension
The development of hypertension in patients with primary malignant brain neoplasms occurs through several distinct mechanisms that reflect the complex interplay between intracranial pathology and cardiovascular regulation:
Increased Intracranial Pressure
Malignant brain tumors often cause elevated intracranial pressure (ICP) due to mass effect, edema, or obstruction of cerebrospinal fluid flow. This increased pressure can stimulate the brainstem’s vasomotor centers, leading to systemic vasoconstriction and increased blood pressure in an attempt to maintain cerebral perfusion pressure—a phenomenon known as the Cushing reflex . This triad of hypertension, bradycardia, and irregular breathing represents a neurological emergency that requires immediate intervention.
Direct Compression of Brain Regions
Tumors located in or compressing specific brain regions responsible for cardiovascular regulation can directly cause hypertension. These regions include:
- The nucleus tractus solitarius in the medulla oblongata
- The ventrolateral medulla
- The hypothalamus
- The insula cortex
Disruption of these areas can impair baroreceptor reflex function and increase sympathetic outflow, leading to sustained hypertension .
Neuroendocrine Effects
Certain primary brain tumors, particularly those located near the pituitary gland or hypothalamus, can disrupt the normal production and regulation of hormones that influence blood pressure, such as:
- Cortisol (through disruption of the HPA axis)
- Catecholamines (through sympathetic activation)
- Vasopressin (antidiuretic hormone)
These neuroendocrine disturbances can contribute to the development of secondary hypertension that may persist even after treatment of the primary tumor .
Clinical Presentation and Diagnostic Considerations
Patients with hypertension secondary to primary malignant brain neoplasms present with a constellation of symptoms that reflect both the underlying tumor and the cardiovascular effects:
Neurological Symptoms
- Headaches that are typically worse in the morning
- Nausea and vomiting unrelated to food intake
- Seizures of new onset
- Focal neurological deficits depending on tumor location
- Visual changes including papilledema
- Cognitive impairment or personality changes
Cardiovascular Symptoms
- Elevated blood pressure readings, often with loss of normal diurnal variation
- Orthostatic hypotension in some cases due to impaired autonomic regulation
- Tachycardia or bradycardia depending on the specific neural structures affected
Diagnostic Approach
The diagnostic workup should include:
- Neuroimaging (MRI with contrast) to characterize the brain tumor
- 24-hour blood pressure monitoring to establish hypertension patterns
- Laboratory studies to rule out other causes of secondary hypertension
- Autonomic testing in selected cases to evaluate cardiovascular regulation
- Endocrine evaluation if hypothalamic-pituitary involvement is suspected
Table: Differential Diagnosis of Hypertension in Brain Tumor Patients
| Condition | Key Features | Distinguishing Tests |
|---|---|---|
| Brain tumor-related hypertension | Associated with neurological symptoms, may have Cushing triad | MRI brain, pattern of BP elevation |
| Essential hypertension | No underlying cause identified, family history | Normal neuroimaging, response to常规 antihypertensives |
| Renovascular hypertension | Abdominal bruit, flash pulmonary edema | Renal artery ultrasound, angiography |
| Primary aldosteronism | Hypokalemia, muscle weakness | Aldosterone-renin ratio, adrenal CT |
| Pheochromocytoma | Paroxysmal hypertension, palpitations | Plasma metanephrines, adrenal imaging |
Treatment Implications and Considerations
The management of hypertension in patients with primary malignant brain neoplasms requires a multidisciplinary approach involving neuro-oncologists, neurologists, cardiologists, and primary care physicians:
Addressing the Underlying Cause
The most effective approach to managing brain tumor-related hypertension involves treating the primary neoplasm through:
- Surgical resection to reduce mass effect and intracranial pressure
- Corticosteroids (e.g., dexamethasone) to reduce peritumoral edema
- Radiation therapy to control tumor growth
- Chemotherapy or targeted biological therapies
Reducing tumor burden and controlling intracranial pressure often lead to improvement in hypertension without requiring additional antihypertensive medications .
Antihypertensive Therapy
When specific antihypertensive treatment is necessary, drug selection should consider the unique pathophysiology of neurogenic hypertension:
- Beta-blockers may be particularly effective due to their ability to reduce sympathetic outflow
- Calcium channel blockers can help manage hypertension without compromising cerebral blood flow
- ACE inhibitors and ARBs may be used but require careful monitoring in patients with potential electrolyte disturbances
- Avoid excessive blood pressure reduction which could compromise cerebral perfusion
Monitoring and Follow-up
Patients require close monitoring of both their oncological and cardiovascular status:
- Regular blood pressure checks with attention to postural changes
- Serial neurological examinations to assess tumor status
- Medication adjustment as the brain tumor responds to treatment or progresses
- Screening for end-organ damage from hypertension (e.g., echocardiograms, renal function tests)
The Importance of Accurate Coding
Proper ICD-10-CM coding for hypertension due to primary malignant brain neoplasms has significant implications beyond reimbursement:
Clinical Care and Research
Accurate coding facilitates:
- Appropriate resource allocation for complex patients requiring multidisciplinary care
- Epidemiological research on the cardiovascular effects of brain tumors
- Clinical trial design with better stratification of patients
- Outcome studies that account for cardiovascular comorbidities
Reimbursement and Healthcare Economics
Precise coding ensures:
- Adequate reimbursement for the increased complexity of caring for these patients
- Justification of resource utilization including advanced imaging and specialist consultations
- Accurate representation of case mix for healthcare institutions
- Appropriate risk adjustment in value-based payment models
Quality Measurement and Reporting
Quality measures increasingly incorporate:
- Comorbidity adjustment in oncology quality metrics
- Documentation of treatment-related complications
- Outcome measures that account for cardiovascular health
FAQs on Hypertension and Brain Tumors
What is the correct ICD-10-CM code for hypertension caused by a primary malignant brain tumor?
There is no single ICD-10-CM code that directly represents “hypertension due to primary malignant brain neoplasm.” Instead, coders should use two codes: C71.9 (Malignant neoplasm of brain, unspecified) and I15.9 (Secondary hypertension, unspecified), with the sequencing dependent on the reason for the encounter . Clinical documentation must clearly establish the cause-effect relationship between the brain tumor and hypertension for appropriate coding.
How do brain tumors cause hypertension?
Brain tumors can cause hypertension through several mechanisms, including: increased intracranial pressure triggering the Cushing reflex; direct compression of brain regions involved in blood pressure regulation (such as the brainstem or hypothalamus); and neuroendocrine effects that disrupt normal hormonal control of cardiovascular function . The specific mechanism depends on the tumor location, size, and type.
Is hypertension in brain tumor patients always considered secondary hypertension?
Not necessarily. While hypertension developing after the diagnosis of a brain tumor is likely secondary to the neoplasm, some patients may have pre-existing essential hypertension (I10) that is unrelated to their cancer diagnosis . The clinical context, timing of hypertension onset, and documentation by the treating physician determine whether the hypertension is coded as essential or secondary.
What additional codes might be needed for complications?
Depending on the clinical scenario, additional codes may be required for complications such as:
I67.4: Hypertensive encephalopathy
I16.1: Hypertensive emergency
Codes for specific end-organ damage (e.g., hypertensive heart disease, hypertensive chronic kidney disease)
Codes for treatment-related effects (e.g., steroid-induced hypertension)
How does treatment of the brain tumor affect hypertension?
Treatment of the primary brain tumor often improves or resolves hypertension that was directly caused by the neoplasm . Surgical decompression, reduction of tumor mass through radiation or chemotherapy, and management of peritumoral edema with corticosteroids can all alleviate the mechanisms causing hypertension. However, some treatments (particularly corticosteroids) may themselves cause or exacerbate hypertension, requiring careful management.
Conclusion
Hypertension secondary to primary malignant neoplasm of the brain represents a clinically significant comorbidity that requires thoughtful management and precise documentation. The ICD-10-CM coding approach necessitates careful application of coding guidelines to accurately represent the relationship between the brain tumor and hypertension. Proper documentation is essential for ensuring accurate coding, appropriate reimbursement, and optimal patient care. As treatment modalities for primary brain tumors continue to evolve, with patients living longer, the cardiovascular sequelae of these tumors and their treatments will become increasingly important aspects of comprehensive neuro-oncologic care. A multidisciplinary approach involving neuro-oncologists, neurologists, cardiologists, and coding specialists is essential for optimizing outcomes for these complex patients.